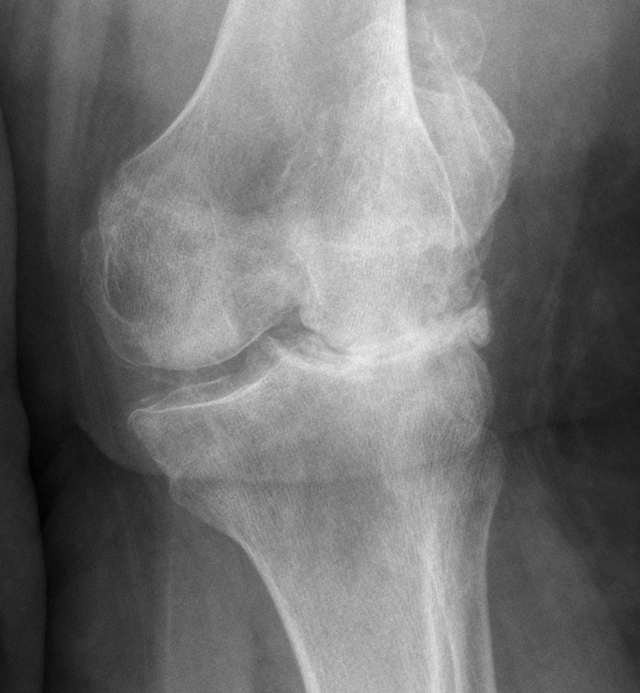
Components Prostheses
- An upper metal component shaped and sized to fit to femur bone contour
- A flat metal tibial component made of metal alloys fixed to the bone
- A plastic insert designed to bear significant wear
- A plastic patella button which resurfaces the back of your knee cap.
Pathway for Simon's Total Knee Patients
Booking in for Surgery
Once you have made the decision to proceed with joint replacement surgery Sylvia, Rochelle or Tash will help you to fill in the appropriate paperwork, and the operation will be booked with the hospital. Usually we will plan a provisional date for surgery at this stage (this can be changed if needed). The SJOG Booking forms need to be taken to the Admissions office at SJOG Hospital as soon as is convenient. The staff in Admissions at SJOG will contact your Health Insurance provider and confirm their approval to proceed. They will also arrange for you to have a pre op nurse assessment.
Pre-Op Nurse Assessment
Admissions will book you in for this at SJOG Hospital. The Pre Assessment Nurse will help answer any questions you may have about the whole process. She will also assess your home situation to ensure you have adequate home support in the first few weeks following surgery. If you live alone it may be necessary to arrange a package of community care to help during the first few weeks at home. The nurse will also give you an antiseptic wash to use on the evening before surgery. Do not shave around the operation site or apply any skin creams in the 48 hours before surgery. Take great care of the skin on your legs (beware of insect bites and gardening scrapes!) as if there is a wound on the leg it may be necessary to delay your surgery.
Pre-Op Tests
You will be given a form for a series of routine tests at the time of booking in my Rooms. These need to be done at Australian Clinical Labs, which is just inside the front entrance of SJOG Hospital. The routine skin swabs for MRSA/MSSA and the routine bloods and urine tests need to be done as soon as possible. No formal booking nor fasting is required for this; you can just present to the Australian Clinical Labs Rooms at SJOG Hospital. The Group and Save blood test may need to be repeated on the day of admission (the admission nurse will organise this) and a form will be provided for this on the day.
Insurance Company
Sylvia, Tash or Rochelle will give you a printed quote of the cost for your procedure. You need to take this quote to your health insurance company and they will let you know what the gap payment (if any) will be. Admissions at SJOG will also confirm that your health insurance company will cover you for your procedure.
Pre-Op Physiotherapy
I believe pre op physiotherapy is worthwhile prior to hip and knee surgery. If you can optimise your range of motion and muscle control prior to surgery, the recovery should be faster and easier post surgery. There is evidence supporting this. Hayley Orsmond is a local physiotherapist who provides pre-operative one on one assessment and exercise consults in our Rooms on a Tuesday afternoon. The cost of these sessions can be claimed from your private health insurance if you have ancillary cover for physiotherapy. Please speak to Sylvia, Rochelle or Tash if you would like to make an appointment to see Hayley. If you live further afield or already have a regular physiotherapist they should also be able to help with this.
Anaesthetic Assessment Prior to Surgery
At the time of booking you will be given a contact for your anaesthetist. I work with several different anaesthetic specialists. Most of the anaesthetic specialists do like to see my patients pre operatively in their Rooms for an anaesthetic assessment. Sometimes the anaesthetist may arrange some further pre op tests although this is not routine
When to Come Into Hospital & When to Stop Eating/Drinking Pre-Op?
The order of the list is not usually formalised until a few days before surgery as emergencies are sometimes added at short notice. You will need to ring SJOG hospital on 97221815 between 11am and 3pm the day before surgery. They will tell you when to stop eating/drinking and what time you need to report to the hospital. Admission is always on the day of surgery.
Day of Surgery
Make sure you shower on the day of surgery. As mentioned above, do not shave around the operation site or apply any skin creams on the day of surgery. Report to the Day Surgery Unit (opposite the Blue Wren café via the SJOG Main Entrance) at the time agreed. Make sure you do not eat or drink unless you have been told to. If you are allowed to drink fluids make sure they are “clear” (no milk). Bring a small bag with some basic provisions for your stay: toiletries, pyjamas, comfortable clothes, phone/charger, reading material. Your bag will be labelled and taken to your Room (it will be there for you when you return to the Ward post operatively) and the Day Surgery staff will admit you to the Day Surgery unit pre operatively. You will be given a hospital gown to change into and then wait in this area until you are called to theatre for your operation. The timing of an operating list is not an exact science and so there is often a wait of a few hours. We appreciate this is not perfect (and apologise in advance if the preop wait ends up being onerous) but it does provide the flexibility required to run an operating list efficiently.
Surgery: Day of Surgery
Hip replacement surgery generally takes about an hour. We routinely use a combination of nerve blocks/spinal anaesthetic and infiltration of local anaesthetic at the operation site. This means the legs are usually numb when you wake up from the anaesthetic in the Recovery Room of theatres and most people are essentially pain free when they wake from surgery. This combination provides excellent pain relief and reduces the amount of strong painkillers required. The numbness slowly wears off over the first 24 hours and then pain relief is given in the form of either regular tablets or a PCIA IV Pump (this is generally decided by the anaesthetist). If the anaesthetist prescribes a PCIA Pump it will allow you to self administer strong pain relief intravenously very simply by pressing a button. This puts you in complete control of how much pain relief that you feel you need. The amount required varies a great deal from person to person. There is a lock out system to ensure that you cannot be given too much. The commonest side effects of the strong painkillers are nausea, itching and constipation although many patients experience little or no problems. If you do have some nausea, let your nurse know and they will arrange for you to have medication for this (called an antiemetic). Anti-histamine tablets usually help with any itching and I now routinely prescribe mild laxatives in the first few days post surgery to help prevent any problems with constipation. A urinary catheter will routinely be placed into your bladder in the theatre by my medical assistant or by one of the nursing staff. This is done while you are asleep and it can usually be removed on the first morning after surgery. Occasionally a small plastic drain is placed at the site of surgery to collect any post surgery bleeding although this is no longer routine.
Surgery: Day 1 Post-Op
I use an ERAS (enhanced recovery after surgery) accelerated rehabilitation programme and on the first morning after surgery we aim for you to complete the following:
- Remove catheter/PCIA/any drains
- Stand up and walk to the bathroom using a frame (with help from your physiotherapist and nurse)
- Shower and change into loose fitting comfortable clothes
By the end of day 1, I aim to have people free of any encumbrances (drain, PCIA, catheter), showered and starting to mobilise.
Surgery: Days 2 & 3
The next few days after surgery are aimed at improving your mobility whilst keeping your pain levels well controlled. Most people find the second day the hardest as the local anaesthetics have all worn off and the inflammatory response to the operation has kicked in. You will be given painkiller tablets to ensure you are comfortable and the physiotherapist will see you each day. A small injection of Clexane is routinely given in to the skin of the abdomen each day to minimalise the risk of a thrombosis (leg clot). The hospital stay is often quite disruptive to your sleep patterns and I am always happy to prescribe sleeping tablets during this period. The wound is either sealed off with a Prineo dressing or a combination of steristrips and a plastic dressing. The Prineo dressing is a Superglue mesh that is strong, water resistant and antibacterial and stays on undisturbed until day 10-14. The stitches are all dissolvable so there are no stitches/clips to remove. Most people are independently mobile on crutches and able to go home on Day 3.
Hydrotherapy/Swimming
Hydrotherapy is available at SJOG and some patients find this helpful. There is no good evidence that it makes any difference to your long term outcome however and I generally leave the choice of whether to do hydrotherapy up to the patient. It can be arranged by liaising directly with the physiotherapy department at SJOG. It is reasonable to get into the hydrotherapy pool (or any pool or the sea) once the wound is healed and dry. 10-14 days is usually about right. Moving around in a pool is ok at this stage but I would avoid swimming for at least 6 weeks (and breast stroke leg kick for 3 months)
First Week Home
Don’t be worried if the leg is bruised and swollen in the first few weeks. There is always bleeding from the bone around the time of surgery and this can slowly migrate down the leg with gravity in the first few weeks. Time, ice and elevation will help. The wound should be dry at this point and if it is not please let me know. You will be given medication to take home with you when you leave hospital. Unless there is a contraindication this usually includes:
Blood Thinner
• The routine recommendation is a small dose of Aspirin once a day for 6 weeks. If you are already taking a tablet to thin the blood prior to admission then I will usually send you home on your usual blood thinner.
Pain relief
• Paracetamol
• Anti inflammatory painkiller (usually Celebrex) • Short-acting strong opiate painkiller (usually Tapentadol IR or Targin)
• Long-acting strong opiate pain killer (usually Tapentadol SR or Buprenorphine)
NB the brand name for Tapentadol is Palexia (ie these are the same medication)
Try and wean off the strong opiate painkillers first, then the anti inflammatories and then the paracetamol last. Anti inflammatories are contra indicated if you have kidney failure or asthma and should be discontinued if you have any indigestion/heart burn symptoms. Bear in mind that the strong opiate painkillers provide powerful pain relief, but side effects include constipation and nausea as well as feeling a bit fuzzy or sleepy. Most hip replacement patients manage to wean themselves off all painkillers in the first 2-6 weeks. It is not uncommon to need regular pain relief for up to 2-3 months after knee replacement surgery. Most GPs are happy to prescribe further medication if you need more. If you do have constipation problems, then simple laxatives such as Dulcolax can be bought from a chemist without a prescription. In more problematic cases a Bisacodyl suppository is usually very effective.
Showering
• You can shower straight away (you will be having a shower on the first morning after your operation). Avoid sitting in a bath during the first 2 weeks.
Exercises/Physiotherapy
• You will be seen daily and given some simple exercises to carry out at home by the physiotherapist prior to discharge. Regular ice packs are helpful for swelling reduction and worthwhile for up to 3 months (especially with knees).
• I recommend seeing a physiotherapist during the second week post op. This is more important for the knees than the hips. The physiotherapist should be able to guide your rehab from there but usually 6-12 weeks is about right with on going self directed exercises after that.
Sleeping
• I am happy for you to sleep in whatever position is comfortable. Often a pillow packed around the leg will help. The knee often aches at night and most patients experience this. It usually settles around the six weeks mark.
Wound Check (10-14 Days Post Surgery)
You should have an appointment to see my practice nurse at the Rooms on the Friday afternoon 10-14 days post surgery. I routinely use a dissolvable suture, which means there are no clips/sutures to remove. The nurse will change your dressing and check that the wound is healing uneventfully and that all is going well. If you live more than 20-30 minutes drive from Bunbury it may be more convenient to see your local GP/practice nurse, which is fine as long as I am informed if there are any concerns. I am able to provide a script for more pain relief medication at this visit if required.
Physiotherapy
I believe physiotherapy is worthwhile in the first 3 months following surgery especially after knee replacement surgery. This can be arranged via SJOG physiotherapy department, with Hayley in our Rooms or with your local physiotherapist.
Six Weeks Check
I routinely see patients about 6 weeks after surgery. This is a brief clinical review to ensure all is progressing well. No X rays are required at this review. If the knee is not bending beyond 90 degrees a “manipulation under anaesthetic” may be considered to stretch the knee and help regain more bend although this is only required in about 5% of patients.
Driving
For surgery on the right leg driving should be avoided for 6 weeks and recommenced once you feel you can safely perform an emergency stop. For surgery on the left leg you can drive an automatic car at 2-4 weeks (when you can comfortably get in and out of the car and are no longer taking strong pain relief medication), and you can drive a manual car at 6 weeks.
Flying
I would not recommend flying in the first 6 weeks after surgery due to the small increased risk of thromboembolic problems (clots) and swelling. If it is necessary to fly then keep well hydrated, keep stretching your legs throughout the flight, wear TEDS stockings and take your blood thinner tablets as prescribed.
Six Months Check
At six months post surgery you will be sent a questionnaire to fill in. Most patients are doing well at this stage and can be discharged. If the score from this questionaire is low or you have any concerns we will arrange a clinical review with a new X ray. In the longer term the Australian Orthopaedic Association recommends a review at about 10 years after surgery with an X ray unless there are any concerns prior to that. I do keep my clinical/outcome data and it is used for audit and research purposes. Please let my staff know if you have any concerns with this. Most knees are going really well at this point but will continue to improve for a further six months. Sometimes there is still mild warmth and swelling in the knee post activity and everyone has a small numb patch on the outside of the knee which is permanent.
Problems
If you have any worries or concerns then please contact Sylvia, Rochelle or Tash at the Rooms. Most minor queries can be dealt with by email/phone. If for some reason we cannot be contacted, then please contact your GP, or for emergencies present directly to ED (there is an orthopaedic team on call 24/7 at BRH ED).