ACL Reconstruction
The Anterior Cruciate Ligament
The anterior cruciate ligament (ACL) is one of the major stabilising ligaments in the knee. It is a strong rope-like structure located in the centre of the knee running from the femur to the tibia.
When this ligament tears unfortunately, it doesn't heal and often leads to the feeling of instability in the knee.
ACL reconstruction is a commonly performed surgical procedure and with recent advances in arthroscopic surgery can now be performed with minimal incisions and low complication rates.
ACL Function
Causes of ACL Tears
Symptoms of ACL Tears
ACL Injury Diagnosis
- Examination reveals instability/laxity of the knee
- MRI (Magnetic Resonance Imaging) invariably confirms the diagnosis and excludes associated injuries.
Initial Treatment Options for ACL Tears
Initial management post injury includes:
- Rest
- Ice
- Elevation
- Compression
Some ACL Injuries do not require surgery particularly in older patients who do not play regular pivoting sports. These patients still need to work on:
- strengthening exercises/physiotherapy
- consider bracing with sports
Indications for ACL Surgery
Suitable candidates for ACL Reconstruction Surgery include:
- Young patients wishing to maintain an active lifestyle
- Sports that involve twisting activities, e.g., soccer, netball, football
- Giving way with activities of daily living.
- Physically demanding occupations, e.g., policemen, firemen, roofers, scaffolders
It is advisable to have physiotherapy prior to surgery to regain motion and strengthen the muscles as much as possible.
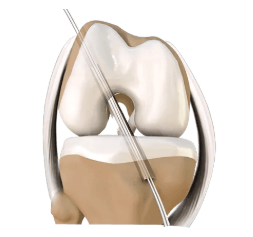
ACL Reconstruction Technique
The surgery is performed arthroscopically. The ruptured ligament is removed and then tunnels in the bone are drilled to accept the new graft. This graft which replaces your old ACL is usually one or two of the hamstring tendons.
The graft is passed through the drill holes in the bone.
The new tendon is then fixed into the bone with various devices to hold it in place while the ligament heals onto the bone (usually 3-4 months).
The rest of the knee can be clearly visualized at the same time and any other damage is dealt with.
The wounds are then closed and a dressing applied.
Early Post-op Steps
Surgery is performed as a day procedure or an overnight stay.
- You will have pain medication
- A nerve block and local anaesthetic is generally used to make sure you are comfortable when you wake from the anaesthetic
- A splint is usually used overnight (until the nerve block wears off)
You will be seen by a Physiotherapist who will teach you to use crutches and show you some simple exercises to do at home.
- Leave any waterproof dressings on your knee until your post-op review.
- You can put all your weight on your leg.
- Put ice on the knee for 20 minutes at a time, at least three times a day
Physiotherapy usually commences after about a week
If you have any redness around the wound or increasing pain in the knee or you have a temperature or feel unwell, you should contact Dr Smith's office or your GP as soon as possible.
ACL Rehabilitation
The early aim is to regain range of motion, reduce swelling and achieve full weight-bearing.
The remaining rehabilitation will be supervised by a Physiotherapist and will involve activities such as exercise bike riding, proprioceptive exercises and muscle strengthening.
Cycling can begin at 2 months and jogging can generally begin at around 3 months. The graft is strong enough to allow sports training at around 6 months. However, other factors come into play such as confidence, fitness and adequate rehab; your physiotherapist can guide you with this.
Recreational athletes usually take 10 -12 months to return to competitive sports.
The rehabilitation and overall success of the procedure can be affected by associated injuries to the knee such as damage to meniscus, articular cartilage or other ligaments.
The following is a more detailed rehabilitation protocol useful for patients and physiotherapists. It is a guide only and must be adjusted on an individual basis taking into account pain, other pathology, work and other social factors.
Post Operative Information
Days 1 and 2
- The knee is not routinely braced or immobilised, although this will depend upon the surgeon’s preference
- Antibiotics will be given in theatre
- Painkillers will be administered on the ward and to take home on discharge. DVT prophylaxis: early foot and leg exercises and mobilisation.
- Swelling control: Ice Packs on Ward
- Full passive extension immediately post-operatively and throughout the hospital stay (use folded pillow under heel when in bed). Static quadriceps exercises.
- When you return to the ward from the recovery unit start moving your operated knee gently (bending and straightening). If this hurts, slow down and rest. Some patient’s may be given a CPM (continuous passive motion) device to help with the movement.
- Weight-bear as able, aided with elbow crutches. Aim to progress to full weight bearing, once you have satisfactory quadriceps muscle control, reasonable gait and good knee extension. Your physiotherapist will guide you with this.
- Start with basic proprioceptive exercises as soon as you start weight-bearing: briefly shift weight on the operated leg and try to balance on one leg (this may be sore and difficult!).
- Reduce bulky dressing to skin dressing only, 24 hours post-operatively
- Active knee bending on sliding board.
- Knee bending whilst sitting, over the edge of the bed.
- Static hamstring exercises at various points in range.
- Static quads in full extension
- Patella mobilisation will be taught by your physiotherapist
- Discontinue any exercise that causes unexpected pain and discuss it with your physiotherapist or surgeon.
PROPRIOCEPTIVE EXERCISES:
Balance and proprioceptive training are very important components of this rehabilitation program. A quick and easy way of doing daily proprioception and balance exercises is to stand on one leg while brushing your teeth. This gives you regular opportunities to exercise proprioception for several minutes, a couple of times each day. Even if you have poor balance and proprioception initially, you can do your exercises whilst holding on to the sink with the opposite hand. As your skill level improves you can progress to “no hands” exercises. The next skill level involves the same exercise but with closed eyes, which may feel strange and will require some practice. Once these exercises become too easy, try to lean in different directions (while standing on one leg and brushing teeth), and then stabilise yourself without losing balance. This will enable you not only to master the skill or standing in one spot, but also to fine-tune the ability to balance once the centre of gravity has moved. Also, remember, that brushing teeth up and down and sideways are very different proprioceptive exercises.
1 to 6 weeks
- Continue to regain full extension with closed kinetic chain exercises (always exercising with weight through the leg). This is the most important target for now!
- Proprioceptive aptitude: improve on balance with eyes shut, shift weight from one leg to other, walk along lines in all directions, catching ball, move ball around foot, use wobble board. Increase one-legged activities.
- Flexion exercises: wall and heel slides. Aim for 90 degrees by the end of second week post-operatively.
- Normalise gait: walk in front of mirror.
- Discard crutches once walking well and confident in activities of daily living.
At 6 weeks
- Continue to progress according to your abilities.
- Progress with closed kinetic chain exercises.
- Hamstrings exercises.
- Dynamic proprioceptive exercises.
- Carefully resume gym work (exercise bike and step machines) as directed by your physiotherapist.
- Swimming: Straight leg kick only (not breaststroke leg action) and pool exercises.
- You should have a full range of movement (symmetrical full hyperextension to full flexion) by the end of this period and minimal or no swelling.
RETURN TO WORK:
This will depend upon your occupation and you should be guided by your physiotherapist and surgeon. It is usual for people with office based jobs to return to work at 2-3 weeks post operatively and more physical jobs such as manual labourers, at about 6 weeks.
DRIVING:
Very little information exists in current literature about the ability of ACL injured or reconstructed knees to respond to situation-specific stimuli, such as braking quickly while driving a car. It is difficult to determine when it is safe to return to driving following surgery. A recent study from Australia seems to indicate that following a right ACL reconstruction, patients should wait at least 6 weeks before driving again. However, this could take place at 2-4 weeks for patients with left ACL reconstruction (or when they are able to operate the clutch if they are driving a manual car).
In all cases, you must be able to safely perform an emergency stop and you should contact your insurance company to ensure you are covered before returning to driving.
FLYING:
There is no universal agreement as to when it is safe to travel by plane after an ACL reconstruction. It seems that most Orthopaedic Surgeons advise their patients not to fly for 4 to 6 weeks following the ACL reconstruction. Short flights do not seem to be a problem. However, long intercontinental flights are a potential problem as there is an increased incidence of spontaneous DVT (deep venous thrombosis), even in the young and healthy passengers. It is possible that sitting for long period of time, in a confined space could predispose to the development of deep venous blood clots, especially in people following recent knee surgery.
If you have to travel by plane, in the first 6 weeks after your ACL reconstruction, you should discuss this with your surgeon
6 to 12 weeks
- At 6 weeks: assessed by surgeon in out patients
- Continue progress: increase gym workouts, step ups and step downs,
- Continue to improve your confidence, gait and proprioceptive aptitude
- Swimming: continue regularly (no breaststroke).
- Cycling on normal cycle.
- Start jogging, on the treadmill, guided by your physiotherapist.
3 to 6 months
- Introduce sport specific exercises.
- Progression of strength work: leg press, leg curls etc.
- Agility work: catching a ball, sideways running, 2 leg jumping, skipping rope etc.
6 to 9 months
- Participating in skill exercises as well as improving power and endurance.
- Return to competitive contact sports is at 12 months provided: no swelling, no ligament laxity, full mobility, full muscle strength and proprioception equal to opposite leg.